Readers are directed to the PDF version of this article, where important additional information can be viewed.
What is a Diabetes UK information prescription?
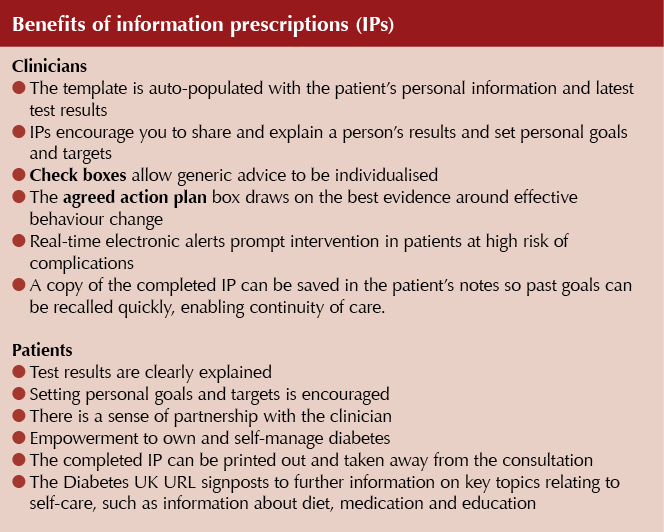
Diabetes UK information prescriptions (IPs) contain personalised easy-to-read explanations, clear images and individual goals to help prevent diabetes health complications. These single-sided A4 sheets are used in clinical appointments. They are built into clinical IT systems, which enables them to be fully integrated with clinical pathways and records. They are designed to give people with diabetes the information they need to understand, engage with and improve on their health targets.
Why are IPs important?
Diabetes is a complex and burdensome disease that requires the patient to make numerous decisions about food choices, physical activity and medications every day. The person needs to acquire a number of self-management skills and have sufficient knowledge and insight into his or her condition to make informed decisions.
IPs are a quick and effective way of engaging people in their diabetes care, increasing understanding and control of their condition. IPs are practical tools that make it easier to have a meaningful conversation with patients about behaviour change.
Once activated in the clinical IT system, the template is auto-populated with the patient’s personal information and test results, leaving the clinician free to spend the consultation time establishing a shared understanding of what matters to the patient and creating a care plan that empowers him or her.
How can you access and activate IPs?
IPs are available within EMIS, Vision and SystmOne. Installation instructions are available at www.diabetes.org.uk/IP-Prof.
Using IPs in the consultation
Experiences of our Editors Pam Brown (EMIS) and Jane Diggle (SystmOne)
- To install and activate the IPs into your clinical system, follow the instructions provided by Diabetes UK.
- In EMIS the IPs are linked to the diabetes template. Provided you tick the box to confirm that you have agreed a diabetes self-management plan with the patient, when you save the template the links to the relevant IPs appear on the screen.
- You can choose which IPs to print in any consultation or not to provide one, if it is felt inappropriate.
- Clicking on the link opens the IP, which self-populates with the patient’s details, including his or her name and GP at the top, and their two most recent results, which personalises the IP making it more relevant for the individual.
- It is useful to understand the parameters the software uses for choosing which IPs to offer. For example, if the patient was diagnosed <8 years ago, the HbA1c IP link appears if the patient’s HbA1c is >48 mmol/mol (6.5%); the link only appears if HbA1c is >58 mmol/mol (7.5%) when the diagnosis was made >8 years ago. However, the facility to personalise the target means advice is still relevant even if we are agreeing a higher target than those triggering the links.
- In SystmOne a link to all eight IPs can be added to the clinical tree and accessed at any point during the consultation. The clinician simply selects the IP that is most relevant to the consultation (though more than one may be completed during the consultation).
- The IPs may be used as a framework for summarising the discussion, encouraging questions and, especially, to encourage patients to participate in setting goals, selecting self-management options and, importantly, agree and record an action plan.
- It helps to summarise the information contained in the IP, agree a target and discuss how this compares with the patient’s previous two readings.
- This can lead into discussions around actions to reduce risk, and boxes on the IP may be ticked.
- Patients can be supported to set personal goals and encouraged to record two steps they will take to achieve these.
- It is an opportunity to highlight that further information is available on the Diabetes UK website and via the link at the bottom of the IP.
- A printed copy should be generated and given to the patient. A copy can also be saved in their clinical record. It is possible to tick a box that will record the fact that the patient has been given a copy of this completed IP.
Further information
You can download activation guides for EMIS Web, Vision and SystmOne or, if your practice uses a different system, information prescriptions from: www.diabetes.org.uk/IP-Prof
Training is available for practices if you email: healthcare@diabetes.org.uk with details of where you are based and your IT operating system.
Endorsements
- “They are hands down the most useful patient resource I have encountered in my diabetes career to date.” Dr Kevin Fernando, GP
- “I’m particularly impressed that they pull in the latest results and allow the clinician to personalise the care plan with the patient. It’s exactly the kind of thing I’ve been looking for as part of the care planning process.” Jane Diggle, Practice Nurse
- “In my own surgery we have seen that the information prescriptions make a big difference both to clinician awareness and patient empowerment. For example, since introducing the kidney disease information prescription, regular audit has shown we have improved the management of those with diabetes and kidney disease and have no-one on contraindicated anti-diabetes medications.” Nicola Milne, Practice Nurse







The mortality benefits of smoking cessation may be greater and accrue more rapidly than previously understood.
2 Apr 2024