Roy Taylor’s recently published book, Life Without Diabetes, can be read in several different ways. Read from cover to cover, it shares Professor Taylor’s research journey to identify how type 2 diabetes develops, the role of liver and pancreas fat in the pathogenesis of the condition, and the clinical studies that eventually led to the DiRECT trial, which demonstrated to the world that diabetes remission is possible and can be maintained at least for two years.
About the book
At its heart, the book describes the new understanding of type 2 diabetes – forget what you learned at medical school! Chapters 1 to 6 set the scene by explaining in detail how the body handles food, and how eating more than is right for an individual can result in excess fat storage in the liver and pancreas, resulting in type 2 diabetes over time. For people who just want to take responsibility for trying to put their type 2 diabetes into remission, Chapter 7 describes the three-step Newcastle weight-loss programme. This programme promotes 8–12 weeks of rapid weight loss using liquid meal replacements, followed by gradual reintroduction of food and then a weight maintenance phase that is ideally continued lifelong. Chapter 8 focuses on the challenging matter of how to maintain weight loss once it is achieved. The recipes that conclude the book are geared to each of the three steps of the programme. Throughout, the book addresses many of the myths around weight loss and obesity.
The three-step weight-loss programme
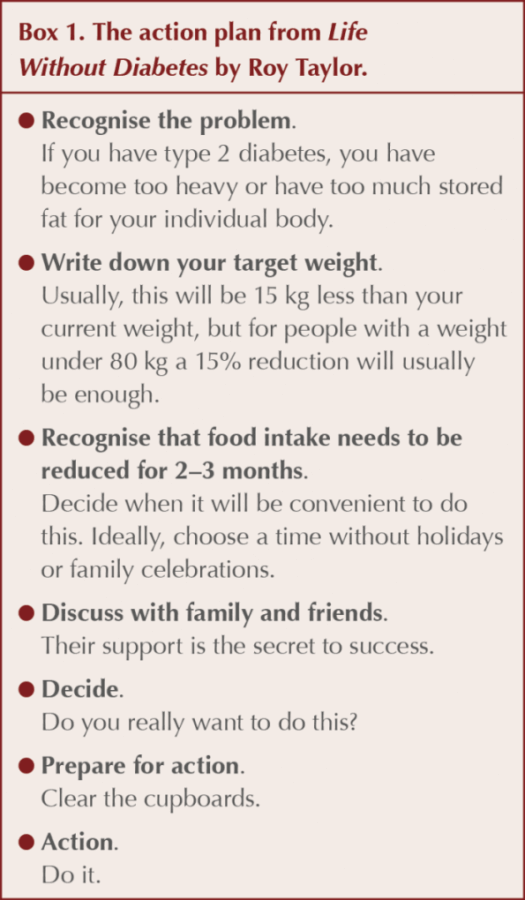
Before the reader embarks on the weight-loss programme, the book provides an action plan to help them to prepare for success (Box 1).
Step 1
Rapid weight loss with a 700–800-calorie/day diet.
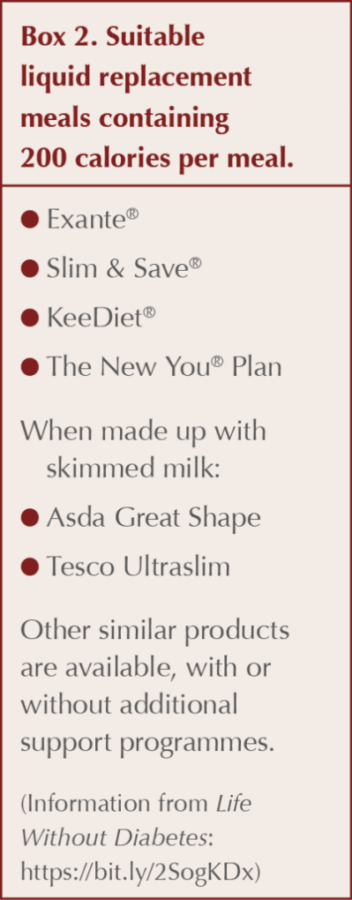
The goal is to achieve a rapid weight loss of 15 kg (or 15% of body weight in people who weigh less than 80 kg). Very low calorie liquid complete nutrition is recommended for this stage – three sachets, each providing 200 calories approximately, and then one small meal of non-starchy vegetables to increase the fibre content and provide something to chew. Although any diet (including “real” food) providing this number of calories is likely to be effective, choice can make adherence more difficult and therefore using a commercial product simplifies the programme. A list of complete meal replacement products from the Newcastle site is shown in Box 2. No alcohol is recommended during this step because of its high calorie content.
People describe loss of hunger after 36 hours on the programme and, since they rapidly lose weight (usually 3.5 kg in week 1), they feel better and more energetic. Interestingly, exercise or high activity levels are not recommended during Step 1 as this triggers increased appetite and compensatory eating. Professor Taylor describes this as one of the lesser known secrets of weight loss.
Although slower weight loss over a longer period will achieve the same metabolic benefits, this is more difficult for most people as hunger is troublesome during lesser calorie reduction and boredom tends to occur, making the 15-kg weight loss harder to achieve and less likely.
Step 2
Gradual reintroduction of normal healthy meals, one meal at a time every 2 weeks.
People describe finding it difficult to make decisions about what to cook and eat after a period on complete liquid meals, so the programme recommends reintroducing one meal every 2 weeks while discontinuing the shakes, and provides recipes for use in this phase. People are warned to expect weight gain of around 1 kg at this stage as their glycogen stores are replenished. Some people find that the 8–12 weeks on the liquid meal replacement diet makes it easier to establish completely new eating habits when food is reintroduced, rather than just trying to modify existing established habits.
Step 3
Weight maintenance
Professor Taylor reminds people that they will only need to eat around three quarters of their previous food consumption to fuel their smaller body and outlines ways that people may choose to achieve this, including a moderate decrease in carbohydrates, restricted time eating or 5:2 intermittent fasting (see key concepts below).
Activity is presented as having a role in weight maintenance and longer duration activity, such as walking or gardening, is recommended as this burns more calories than short duration, higher intensity exercise. The latter might be considered for improving heart health, but that is not the primary goal here. The weight change itself produces a drastic decrease in QRISK score.
The underlying science and key concepts
Key concepts discussed include:
- The twin cycle hypothesis – the liver cycle and the pancreas cycle (Figure 1). These are the most difficult concepts within the book to understand for both lay and professional readers, but they underpin the remission process. They are supported by robust clinical evidence and imaging. Weight loss reversing the fat deposition in the pancreas allows the beta cells to revive and restart the production of insulin, resulting in remission or improved blood glucose levels.
- Personal fat threshold. Developing type 2 diabetes means that the individual has exceeded their personal fat storage threshold in their subcutaneous stores, resulting in excess fat being deposited in their liver and pancreas. This explains why not everyone who develops type 2 diabetes is obese – they just have accumulated more fat than their personal threshold. Equally, it helps us explain why those with a higher personal fat threshold may not develop type 2 diabetes despite being morbidly obese. Removing that fat by weight loss can reverse the process whatever the starting BMI and put type 2 diabetes into remission.
- Restricted time eating. This involves eating all food within a limited period each day (e.g. first meal at 12 noon and last meal at 6 pm, resulting in fasting for 18 hours). This can be adapted to the pattern that most suits the person. For example, they could choose to skip breakfast (as in the example), eat earlier in the evening or only eat breakfast and lunch. This may be useful for weight maintenance.
- 5:2 intermittent fasting. This involves eating healthy meals on five days of the week and eating 500–600 calories on the other, non-consecutive two days. There are many resources that help people achieve such low calorie counts on the designated days. This model has the advantage of flexibility and can be less daunting than dieting every day, as the person is never more than 24 hours from being able to eat normally. Once weight loss is achieved and stable, 6:1 intermittent fasting may be effective for weight maintenance. This, too, may be useful for the lifelong weight maintenance phase.
Safe support
As with any good book on medical topics, Professor Taylor reminds people with diabetes to talk first to their primary care team. Information (available at https://bit.ly/38nmd2S) provides guidance for the whole primary care team on when not to use this approach, additional monitoring required, how to manage medication safely (particularly sulfonylureas and insulin), and the importance of monitoring complications (especially retinopathy, as sudden blood glucose changes are likely). Healthcare professionals are reminded that this approach should not be used by those with pancreatic diabetes, monogenic diabetes or slow-onset type 1 diabetes. Armed with this information, we can encourage people and help them stay safe if they choose to undertake this programme.
Our responsibility
This book brings clarity to the physiology and to the simple (although not easy) steps that people can take if putting their type 2 diabetes into remission is their goal. With the DiRECT results, support of organisations such as Diabetes UK and the Primary Care Diabetes Society, ongoing NHS programmes in Scotland and England, and this book being available for people with type 2 diabetes, I believe we now have a responsibility to discuss remission and how it may be achieved with everyone who presents with new type 2 diabetes in our day-to-day practice, as well as at reviews with those in the early years of their type 2 diabetes journey. Those involved in the DiRECT study had had type 2 diabetes for less than 6 years, and all were on oral therapies only, but there have been documented successes in those with more long-standing disease and even those on insulin.
Removal of fat from the liver using an approach such as this may also help stabilise or reverse non-alcoholic fatty liver disease, which is highly prevalent in those with type 2 diabetes. Even if remission is not achieved, the benefits of any weight loss in helping people feel better and having better control of type 2 diabetes would surely make the 12 weeks of the programme a worthwhile investment for motivated people.
This book should be required reading for all of us who manage type 2 diabetes and not just people with the condition. By better understanding the twin cycle hypothesis, and how people can achieve rapid weight loss and weight maintenance, we may be able to support many people to put their diabetes into remission. In a time of escalating new diagnoses of type 2 diabetes, surely we should now consider this as an important part of our role.







The mortality benefits of smoking cessation may be greater and accrue more rapidly than previously understood.
2 Apr 2024