In 2012, the NHS in England introduced the paediatric diabetes Best Practice Tariff (BPT) in a bid to improve care and outcomes for children and young people (CYP) with diabetes. Prior to 2011, paediatric diabetes had not even been recognised as a specialty area and paediatric diabetes clinics were coded as ‘general paediatrics’. Outcomes for CYP were poor compared to our European counterparts and fewer than half of all paediatric diabetes units submitted data to the National Paediatric Diabetes Audit (NPDA). We could not even say with certainty how many CYP with diabetes in England there actually were! Centres were understaffed and poorly resourced, with no guarantee that the clinicians responsible for delivering paediatric diabetes care had even received formal training in that area.
Encouraging and rewarding excellence
Before the BPT was introduced, NHS services in England were funded using a nationally-mandated tariff system for in- and outpatient attendances, which were allocated according to specialty. The BPT system was designed to encourage and reward excellence by setting out standards of care for conditions that, if met, would result in enhanced funding. Looking at European centres of excellence and paediatric diabetes services within the UK that were achieving good outcomes, criteria were drawn up to set out what these standards of care should look like for CYP with diabetes. This included specifying who should be part of the paediatric diabetes team (doctors, nurses, dietitians, psychologists and administration staff as a minimum) and standards of training for all healthcare professionals working within these services. The paediatric diabetes BPT set out:
- Minimum standards for how often these CYP should be seen in clinic
- The importance of additional contacts in between appointments
- The need to provide 24-hour access to emergency advice.
It also recognised the need for clear policies for safeguarding and transition to adult diabetes services in due course.
The BPT mandated that data should be submitted to the NPDA every year, which meant that units could benchmark their performance against other units within their region and nationally. Each paediatric diabetes unit also had to participate in their local CYP Diabetes Network. These regional networks meet three to four times a year. The BPT states that units must attend at least 75% of all CYP Diabetes Network meetings. Every year, each unit presents its NPDA results at its local CYP Diabetes Network meeting, along with an action plan for the following year to address any areas that require improvement.
The decision was made that the BPT would be awarded as a ‘year of care’ payment, with services receiving a fixed remuneration per young person per year, providing the BPT criteria had been met. These standards were also used as the foundation for the national quality improvement programme, which was introduced in England shortly after the BPT came in.
Wales has different funding mechanisms for the provision of NHS services and so did not introduce a BPT. However, Welsh paediatric diabetes services use the same standards to benchmark themselves against and joined the quality improvement programme in 2014.
Changes following BPT introduction
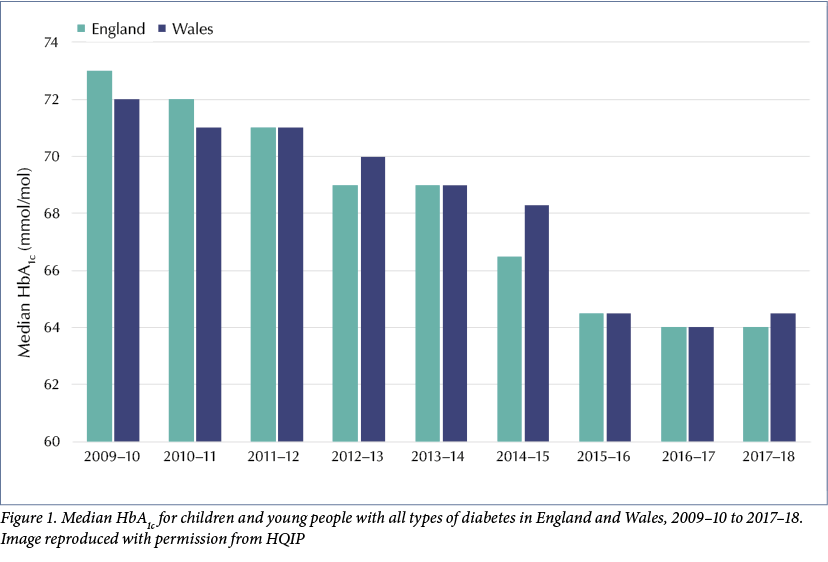
Since 2012, virtually every paediatric unit in England and Wales has submitted data to the NPDA. We now know that there are nearly 30,000 CYP being cared for by paediatric diabetes services in England and Wales, the majority of whom have type 1 diabetes. In that time, the median HbA1C has fallen year-on-year from 70 mmol/mol (8.6%) in 2010–11 to 64 mmol/mol (8%) in 2016–17, see Figure 1. The median HbA1C for 2017–18 was the same as in 2016–17; this is the first year since the BPT has been introduced that there has not been a national fall in HbA1C.
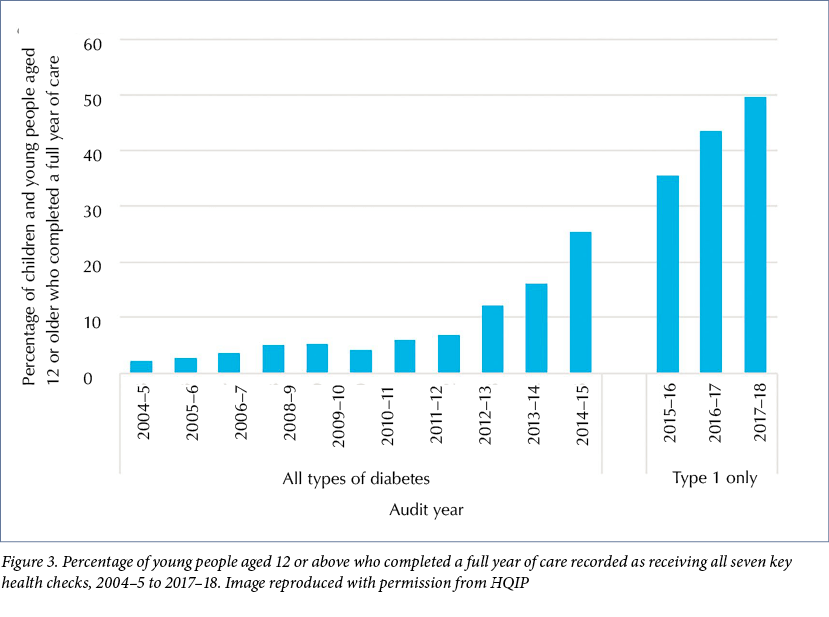
Importantly, the number of units where the mean HbA1C is 75 mmol/mol or above (9% or above) has fallen from 58 in 2011–12 to four in 2017–18. The percentage of CYP with an HbA1C >80 mmol/mol (>12.5%) has also fallen: from 25% in 2011–12 to 16.5% in 2017–18. In that same time period, the percentage of CYP in whom all seven care processes have been recorded as completed has risen from under 10% (Royal College of Paediatrics and Child Health, 2012) to just under 50% (Royal College of Paediatrics and Child Health, 2019), see Figure 2 and Figure 3.
It also appears that admission rates have fallen, with just under 13% of CYP in England and Wales having a diabetes-related admission in 2017–18, compared with nearly 25% between 2012 and 2015. The NPDA data for 2018–19 are awaited and should be published in the next few months.
BPT funding: Benefits and challenges
Since 2012, every paediatric diabetes service in England meeting the criteria has been eligible to claim the BPT payment, which has been just under £3,000 per patient since it was introduced. This was a big increase in overall funding at the start and allowed services to invest in personnel and training to ensure they would be able to meet the standards. From 2014 onwards, this payment included the cost of any inpatient stay due to diabetes (other than the initial admission at diagnosis), regardless of how many times someone was admitted in a year; effectively, this was a decrease in funding, as previously admissions were paid for separately. Added to this, the lack of increase in BPT payment in the past 7 years means that there has been >25% decrease in funding in real terms.
It has long been recognised that just because a trust claims BPT, it does not mean that all the money goes to paediatric diabetes services. This problem has been compounded over the past 1–2 years, as an increasing number of trusts have started negotiating block contracts with commissioners for Clinical Commissioning Group-commissioned paediatric services, which includes paediatric diabetes. This can mean that funding for paediatric diabetes gets swallowed up in the overall funding for general paediatrics, making it harder for services to negotiate replacements for staff members who leave, for example.
Having said all this, NHS England has recognised the hugely positive impact that the BPT has had in improving paediatric diabetes outcomes and, at present – while BPTs still exist as payment systems overall – there are apparently no current plans to remove the paediatric diabetes BPT.
Improving the care of young adults
NHS England has recognised that outcomes for young adults with diabetes are now lagging far behind paediatric diabetes outcomes. Obtaining national data for young people with diabetes aged 16–25 is challenging, as their data are submitted as part of the National Diabetes Audit (NDA) and this does not sub-divide outcomes according to age in younger people; the age bands for the NDA are: <40; 40–64; 65–79; and 80 years and over.
The NHS Long-Term Plan now specifically talks about the importance of seamless services for CYP aged 0–25 years (NHS, 2019a). This is in part in acknowledgement that there is good scientific evidence that brain maturation continues until at least the age of 25 – and longer in young people with poorly-controlled diabetes (Colver and Longwell, 2013). It is thus disappointing that this fundamental difference is not picked up by the age bands in the NDA; most 22-year-olds behave and think very differently from 39-year-olds, with entirely different priorities and focus in life.
Worrying findings in practice
Local and national data on young people in practice highlight a number of areas of diabetes care that need improvement.
HbA1C frequently increases in young adults. Looking at local data in Nottingham, the mean HbA1C in CYP aged 0–19 (including those in the transition clinic) attending the paediatric diabetes service in 2017–18 was 57 mmol/mol (7.4%). For 16–25-year-olds attending the young adult service it was much higher, at 74 mmol/mol (8.9%). Data from primary care colleagues in the North East of England showed that, of those young people aged 16–25 years with an HbA1C recorded in their GP records in the past 12 months, nearly 40% had one >80 mmol/mol (9.5%) reading and <15% had one measurement <58 mmol/mol (7.5%).
Between October 2017 and September 2019, 157 young people aged 16–25 years attended Nottingham University Hospitals NHS Trust emergency department – without necessarily being admitted – due to a diabetes-related problem. The vast majority of these problems were potentially avoidable. Sadly, between September 2015 and October 2016, five young people aged 17–25 years died as a result of diabetes.
In 2012–13, a third of all diabetic ketoacidosis admissions in England were in young people aged 16–25 years, most of which were preventable. The National Diabetes Transition Audit 2011–17 (NHS, 2019b) showed deterioration in the completion of annual care processes, achievement of treatment targets and higher rates of diabetic ketoacidosis in young people who moved from paediatric to adult services. Northampton has shown that attendance rates at clinic appointments halve once young people move from paediatric services, through transition and into young adult clinics.
Proposal for a young adult BPT
The reasons for the deterioration in engagement with services and clinical outcomes in young adults are multifactorial, but it cannot be ignored that young adult diabetes services are substantially less well resourced in terms of staffing, clinic availability, access to technology, etc, than paediatric services. NHS England is working with the Getting It Right First Time project to look at whether a BPT for young adults would be feasible and, if so, what should it look like. There is going to be no additional money for a young adult BPT. However, if it can be demonstrated how much the NHS is currently spending on this cohort due to emergency and unscheduled admissions and contacts, then maybe this money could be redirected to allow commissioners to fund services up front and improve future outcomes. If a pathway and finance can be agreed, then it is hoped that a BPT for young adults may come in from 2021.
Conclusion
The introduction of the paediatric BPT in 2012 and quality improvement programmes leading on from it have resulted in a substantial improvement in paediatric diabetes care and outcomes. We now need to see whether it is possible to duplicate this success with services for young adults.
Acknowledgements: Thank you to Dr Beth Marfleet, GP and clinical lead for diabetes, Hambleton, Richmondshire and Whitby CCG, and Dr Anne Smith, consultant paediatrician at Northampton General Hospital, for sharing their data.






NHSEI National Clinical Lead for Diabetes in Children and Young People, Fulya Mehta, outlines the areas of focus for improving paediatric diabetes care.
16 Nov 2022